CDC Issues New COVID-19 Booster Shot Guidelines for High-Risk Individuals

Anúncios
The Centers for Disease Control and Prevention (CDC) has issued revised guidelines for COVID-19 booster shots, primarily recommending them for individuals at elevated risk of severe illness, reflecting an evolving understanding of immunity and viral variants.
Anúncios
In a significant update signaling an evolving public health strategy, the Centers for Disease Control and Prevention (CDC) has released new guidelines concerning COVID-19 booster shots. These new recommendations specifically target and prioritize individuals identified as high-risk, a move reflecting a refined understanding of the virus’s trajectory and the efficacy of current vaccines.
Understanding the Evolution of Booster Shot Guidance
The landscape of COVID-19 vaccination and booster recommendations has continuously evolved since the pandemic’s onset. Initially, the focus was on broad primary vaccination, followed by general booster recommendations. However, as the virus mutated and population immunity diversified, public health agencies adapted their strategies.
The Centers for Disease Control and Prevention (CDC) plays a pivotal role in this adaptation, constantly monitoring scientific data, vaccine effectiveness against new variants, and the needs of specific population segments. This dynamic approach ensures that guidelines remain relevant and effective.
Anúncios
From Universal to Targeted Recommendations
Early booster campaigns often targeted a wide swathe of the vaccinated population, based on the initial understanding of waning immunity. But as more data became available, it became clear that not all individuals faced the same level of risk or experienced the same decline in protection. This led to a more nuanced view, distinguishing between those who benefited most from additional doses and those for whom the benefit was marginal.
- Initial booster recommendations aimed at broader population coverage.
- Emergence of new variants necessitated constant re-evaluation of vaccine effectiveness.
- Data on waning immunity varied significantly across different age groups and health conditions.
The shift towards targeted recommendations is a testament to the scientific process at work. It emphasizes a data-driven approach, acknowledging that a one-size-fits-all solution may not always be the most efficient or equitable. This evolution not only optimizes vaccine resources but also helps to build public trust by demonstrating a commitment to responsive, evidence-based policy making.
This latest update from the CDC is a prime example of this ongoing refinement. It underscores the agency’s commitment to providing clear, actionable advice based on the most current scientific understanding, ultimately aiming to protect the most vulnerable without over-vaccinating lower-risk groups unnecessarily.
Who are the High-Risk Individuals? Defining the Criteria
Identifying “high-risk individuals” is central to the new CDC guidelines for COVID-19 booster shots. This designation is not arbitrary but is based on a comprehensive assessment of various factors that increase an individual’s susceptibility to severe COVID-19 outcomes, including hospitalization and death. These criteria are meticulously reviewed and updated by public health experts.
The categorization helps to prioritize vaccine distribution and ensures that those who stand to benefit most from an additional layer of protection receive it promptly. Understanding these criteria is crucial for individuals to assess their own risk level and make informed decisions about booster shots.
Key Factors Determining High-Risk Status
Several underlying health conditions, age groups, and occupational exposures contribute to an individual being classified as high-risk. These factors often compromise the immune system’s ability to mount a robust response to the virus or increase the likelihood of exposure.
- Age: Older adults, particularly those over 65, are consistently identified as high-risk due to age-related changes in the immune system.
- Underlying Medical Conditions: Chronic diseases such as severe heart conditions, chronic lung diseases, diabetes, obesity, and kidney disease significantly elevate risk.
- Immunocompromised Individuals: People with weakened immune systems due to medical conditions (e.g., HIV, cancer, organ transplant recipients) or medications are especially vulnerable.
- Certain Disabilities: Individuals with intellectual and developmental disabilities are also considered at higher risk for severe outcomes.
- Occupational and Residential Settings: People living in or working in settings where exposure is high, such as long-term care facilities or healthcare settings, may also be prioritized.
The CDC’s emphasis on these groups reflects a strategic effort to mitigate the most severe impacts of COVID-19. By focusing on those with weakened immune responses or increased exposure, the guidelines aim to create a stronger protective barrier around the segments of the population that are most vulnerable. This targeted approach is designed to maximize public health benefit while optimizing resource allocation in vaccination efforts.
It’s important for individuals to consult with their healthcare providers to understand how these criteria apply to their personal circumstances. Self-assessment can be a good starting point, but professional medical advice ensures that decisions about booster shots are tailored to individual health profiles.

Rationale Behind the Targeted Approach for Booster Shots
The decision by the CDC to narrow its focus for COVID-19 booster shots to high-risk individuals is rooted in a multifaceted scientific and public health rationale. This strategy goes beyond simply recommending more doses; it reflects a sophisticated understanding of immunology, epidemiology, and resource management. It’s a pragmatic evolution that balances individual protection with broader public health objectives.
This targeted approach is not a dismissal of the vaccine’s importance for the general population but rather a strategic shift towards precision in public health interventions. It acknowledges that vaccine immunity varies, that the virus continues to evolve, and that resources are best utilized where they can achieve the greatest impact in preventing severe illness and death.
Scientific Principles Guiding the New Guidelines
At the core of the CDC’s updated recommendations are several key scientific principles. These principles have been refined over the course of the pandemic as more data became available from global studies, clinical trials, and real-world vaccine effectiveness research. Understanding these underpinnings provides clarity on why the guidelines have shifted.
- Waning Immunity: While primary vaccination offers robust initial protection, studies have shown that antibody levels can decrease over time, leading to reduced effectiveness against infection, particularly with new variants. However, protection against severe disease often persists longer.
- Variant Evolution: The emergence of new SARS-CoV-2 variants, such as Omicron subvariants, has demonstrated altered transmissibility and immune evasion properties. Boosters formulated to target newer strains are crucial for maintaining protection against current circulating viruses.
- Immunological Response in Vulnerable Populations: High-risk individuals, including the elderly and immunocompromised, often have a less robust or durable immune response to initial vaccination. An additional dose can help “top up” their immunity to a more protective level.
- Risk-Benefit Analysis: For healthy, lower-risk individuals, the benefit of an additional booster may be less pronounced compared to the potential for mild side effects, especially if they have already experienced natural infection or multiple vaccine doses. The focus shifts to preventing severe outcomes rather than mild infections.
Furthermore, the CDC’s approach considers the overall burden on healthcare systems. By preventing severe illness in those at highest risk, the guidelines aim to reduce hospitalizations and demand for intensive care resources, thereby safeguarding healthcare capacity. This not only protects the individual but also supports the entire community.
The underlying message is clear: while vaccination remains paramount for all eligible individuals, booster strategies must be dynamic, reflecting the latest science and targeting interventions where they are most critically needed. This strategic thinking helps ensure the ongoing effectiveness of public health initiatives against a constantly changing viral threat.
Impact on Public Health and Vaccine Accessibility
The CDC’s new guidelines for COVID-19 booster shots, with their strong emphasis on high-risk individuals, are poised to have a significant impact on both public health outcomes and the accessibility of vaccines. This shift represents a strategic deployment of resources and a refined approach to population-level immunity, aiming to maximize effectiveness where it is most needed.
From a public health perspective, targeting boosters to the most vulnerable populations is expected to reduce rates of severe disease, hospitalizations, and deaths, easing the burden on healthcare systems. Simultaneously, it allows for a more efficient allocation of vaccine doses, potentially improving access for those prioritized groups.
Ensuring Equitable Access for High-Risk Groups
A key challenge and opportunity with targeted recommendations is ensuring that the identified high-risk individuals can easily access the booster shots. This requires clear communication, robust distribution networks, and equitable policies that remove barriers to vaccination. Health equity is paramount in this phase of the pandemic response.
- Clear Communication Campaigns: Public health agencies must clearly articulate who qualifies as high-risk and why booster shots are critical for them. This includes reaching diverse communities through culturally sensitive and accessible information.
- Expanded Access Points: Vaccinations should be available in a variety of convenient settings, including pharmacies, community clinics, physician offices, and mobile vaccination units, to ensure geographic accessibility, especially in underserved areas.
- Addressing Socioeconomic Barriers: Efforts must be made to overcome barriers such as cost (though vaccines are generally free), lack of transportation, and time off work. Policies supporting paid leave for vaccination can play a vital role.
The impact on vaccine accessibility also extends to global considerations. If booster recommendations are more focused, it could potentially free up vaccine supplies for primary vaccination efforts in lower-income countries, contributing to global health equity. However, domestic needs for high-risk groups remain the primary driver for U.S. policy.
Ultimately, the success of these new guidelines hinges on effective implementation and public understanding. While the scientific rationale supports a targeted approach, the real-world benefit will depend on how well these recommendations translate into increased protection for the individuals who need it most, without inadvertently creating new disparities in vaccine access.
What High-Risk Individuals Should Do Next: Practical Steps
For individuals identified as high-risk under the new CDC guidelines, understanding the practical next steps is crucial. This isn’t just about knowing you’re eligible; it’s about actively pursuing the protection offered by the booster shot. Taking proactive measures can significantly bolster your defense against severe COVID-19 outcomes.
The process of getting boosted is generally straightforward, but it requires individuals to be informed and to engage with their healthcare providers and local public health resources. The goal is to make informed decisions that align with personal health circumstances and the latest public health advice.
Guidance for Receiving Your Booster Shot
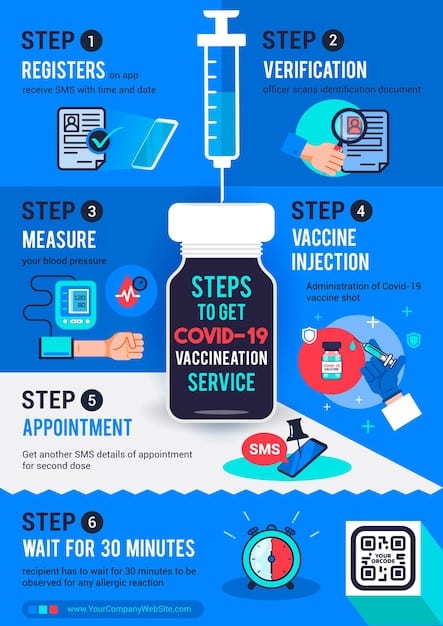
The pathway to receiving a COVID-19 booster shot for high-risk individuals involves a series of steps designed to ensure both eligibility and accessibility. This often begins with direct engagement with the healthcare system and staying informed about local vaccination opportunities.
- Consult Your Healthcare Provider: The first and most important step is to discuss your individual health situation with your doctor. They can confirm if you meet the high-risk criteria and advise on the most suitable booster for you, considering your medical history and current medications.
- Stay Informed on Vaccine Availability: Check local health department websites, pharmacy chains, and the CDC’s VaccineFinder tool for information on where booster shots are available in your area. Appointment scheduling may be required.
- Understand the Type of Booster: Be aware that updated boosters target newer variants of the virus. Your healthcare provider or the vaccine administrator can guide you on which booster is appropriate for you.
- Prepare for Your Appointment: Bring your vaccination record card. Wear loose clothing that allows easy access to your upper arm. Be ready to wait briefly after vaccination for observation.
- Continue Protective Measures: Even after receiving your booster, continue to follow general public health guidance, such as practicing good hand hygiene, considering masking in crowded indoor settings, and staying home when sick, especially if you remain in a high-risk category.
It’s important to remember that these guidelines are designed to offer optimal protection. For high-risk individuals, a booster shot is a key component of a comprehensive strategy to live safely with COVID-19. Proactive engagement with these recommendations is a personal health priority that also contributes to broader community well-being.
Should you have any concerns about potential side effects or specific health conditions, your healthcare provider is the best resource for personalized advice. They can help navigate any complexities and ensure that your booster decision is well-informed and beneficial.
Distinguishing the New Recommendations from Previous Guidelines
The evolution of COVID-19 booster shot recommendations, from broader eligibility to a more targeted approach, marks a significant shift in public health strategy. Understanding the specific differences between these new guidelines and previous ones is essential for both the public and healthcare providers. It highlights a maturing understanding of the virus and vaccine efficacy.
Previous guidelines often emphasized bolstering immunity across a wider age range and for more general populations after a certain time interval from primary vaccination. The current update, however, distills that advice to prioritize specific cohorts, reflecting a more precise risk assessment.
Key Differences in Eligibility and Rationale
The starkest contrast lies in who is now primarily recommended for a booster and the underlying reasoning. This precision reflects advancements in immunological data and epidemiological trends.
- Previous Broad Eligibility: Earlier on, boosters were recommended for most adults after a set period (e.g., six months) following their primary series, sometimes including younger age groups as well. The rationale was to simply raise antibody levels across the population.
- New Targeted Focus: The latest guidelines explicitly narrow the primary recommendation to “high-risk individuals.” This includes older adults, those with specific underlying health conditions, and immunocompromised people. The core rationale is to prevent severe disease, hospitalization, and death in those most vulnerable, rather than just preventing any infection.
- Consideration of Hybrid Immunity: The new guidelines implicitly acknowledge the role of “hybrid immunity” (immunity from both vaccination and prior infection). For many healthy individuals, prior infection coupled with vaccination may provide sufficient protection against severe outcomes, thus reducing the need for an additional booster at this time.
- Variant-Specific Formulations: While not exclusively new, the emphasis on updated booster formulations (e.g., bivalent vaccines) that target currently circulating variants is more pronounced. Previous boosters might have been based on the original SARS-CoV-2 strain.
This strategic shift also signals a move towards viewing COVID-19 management in a manner more akin to influenza, where annual or targeted vaccinations are common. It indicates a transition from an emergency phase to a long-term management phase of the virus. The revised guidelines are designed to offer protection where it counts most, optimizing public health efforts and vaccine deployment.
It’s crucial for individuals not to interpret the narrower recommendations as a sign that vaccines are less important overall, but rather that the strategy for their deployment has become more sophisticated and data-driven to address the current stage of the pandemic effectively.
Future Outlook: Continuous Adaptation and Monitoring
The release of these new CDC guidelines for COVID-19 booster shots is not an endpoint but rather another step in an ongoing, adaptive public health response. The future of COVID-19 management will undoubtedly involve continuous monitoring, scientific research, and policy adjustments. This dynamic approach is critical in the face of an evolving virus and a growing body of scientific knowledge.
Public health agencies worldwide, including the CDC, are committed to remaining agile and responsive. This means frequently reassessing vaccine effectiveness, tracking new variants, and adapting recommendations to ensure the most effective protection strategies are in place for the population.
The Role of Surveillance and Research
Ongoing surveillance and research are the cornerstones of future public health policy regarding COVID-19. Without robust data collection and analysis, it would be impossible to make informed decisions about future booster campaigns or other mitigation strategies. This involves several critical areas of focus:
- Variant Tracking: Continuous genomic sequencing of circulating SARS-CoV-2 strains is essential to identify new variants that might evade existing immunity or cause more severe disease. This informs vaccine updates.
- Vaccine Effectiveness Studies: Real-world efficacy studies are vital to understand how current vaccines and boosters perform against new variants, in different age groups, and among various risk populations over time.
- Immunology Research: Deeper understanding of immune responses, including the durability of vaccine-induced immunity versus natural immunity, will inform future dosing schedules and specific recommendations.
- Burden of Disease Monitoring: Tracking hospitalization rates, ICU admissions, and deaths related to COVID-19 continues to be crucial to gauge the pandemic’s impact and the effectiveness of interventions.
Looking ahead, it’s plausible that future booster recommendations might become even more personalized, potentially relying on individual immune response assessments or more frequent, seasonal updates tailored to prevailing variants, similar to annual flu shots. The long-term goal is to integrate COVID-19 management into routine public health practices, ensuring that interventions are proportionate to the risk and effective for the population segments most in need.
The public should anticipate that guidelines may continue to evolve. Staying informed through official sources like the CDC and consulting with healthcare professionals will remain the best way to navigate these ongoing changes and make the most effective decisions for personal and community health.
| Key Point | Brief Description |
|---|---|
| 🩺 Targeted Focus | New CDC guidance prioritizes high-risk individuals for booster shots. |
| 👴 High-Risk Criteria | Includes elderly, immunocompromised, and those with specific chronic conditions. |
| 🔬 Scientific Rationale | Aimed at preventing severe illness based on waning immunity and variant evolution. |
| 🌐 Public Health Impact | Optimizes vaccine use and reduces burden on healthcare systems. |
Frequently Asked Questions About Booster Shots
High-risk individuals typically include those aged 65 and older, individuals with weakened immune systems due to medical conditions or medications, and people with severe underlying chronic diseases such as heart disease, lung conditions, diabetes, and obesity. Always consult your healthcare provider to confirm your specific eligibility based on your health profile.
The new CDC guidelines primarily focus on recommending boosters for high-risk individuals. For those not in a high-risk group, the decision to get a booster depends on many factors, including the latest circulating variants, individual risk tolerance, and personal health circumstances. Discuss this with your doctor for personalized advice, as general recommendations may vary.
Yes, the latest booster formulations, often bivalent vaccines, are designed to target more recent COVID-19 variants, such as Omicron subvariants, in addition to the original strain. This updated composition aims to provide broader and more effective protection against currently circulating versions of the virus, enhancing your immune response against potential infection.
High-risk individuals can typically receive their booster shots at various accessible locations. These include local pharmacies (such as CVS, Walgreens, Rite Aid), community health centers, primary care physician offices, and public health clinics. Checking the CDC’s VaccineFinder tool or your local health department’s website can provide specific locations and appointment scheduling options.
The frequency of future COVID-19 booster shots for high-risk individuals is still a subject of ongoing scientific evaluation and may transition to a pattern similar to annual flu shots. The CDC continuously monitors data on viral evolution and vaccine effectiveness. It’s best to stay informed through official public health channels and consult your doctor for the most current recommendations applicable to your situation.
Conclusion
The CDC’s updated guidelines for COVID-19 booster shots, with their focused recommendation for high-risk individuals, represent a strategic evolution in public health response. This shift underscores a sophisticated understanding of an ever-changing virus and the imperative to precisely allocate protective measures where they are most impactful. By prioritizing those most vulnerable to severe outcomes, the CDC aims to bolster population-level immunity efficiently, reduce the burden on healthcare systems, and continue navigating the pandemic with a data-driven approach. For high-risk individuals, these guidelines are a critical affirmation of the continued need for proactive vaccination to safeguard health. As the scientific landscape continues to unfold, staying informed through reputable sources and consulting healthcare professionals will remain paramount for all.





